Can Stress and Anxiety Cause Sciatica
Can stress and anxiety cause sciatica? Discover the link between anxiety and sciatica. Learn how to manage and improve the quality of life. Dive in now! As someone passionate about sciatica health and eager to provide helpful suggestions, I understand the frustration and pain that comes with this condition. Sciatica, characterized by radiating pain along the sciatic nerve, can be debilitating and significantly impact daily life. Over time, I’ve come to realize that stress and anxiety can play a significant role in exacerbating sciatica symptoms, making it essential to address these factors to manage the condition effectively.
Understanding Sciatica Pain
Before delving into the relationship between stress, anxiety, and sciatica, let’s first grasp the basics of this condition. Sciatica occurs when the sciatic nerve, which runs from the lower back down the back of each leg, becomes compressed or irritated. This compression leads to a range of symptoms, including sharp pain, numbness, tingling, and weakness along the nerve pathway.
Living with sciatica means navigating through bouts of intense discomfort, making even simple tasks like sitting or walking a challenge. The pain can be relentless, disrupting sleep, work, and leisure activities and impacting overall quality of life.
Does Stress Or Anxiety Cause Pain
The Connection Between Stress, Anxiety and Sciatica
Stress and anxiety are ubiquitous in today’s fast-paced world, but their effects extend far beyond mental well-being. When we experience stress or anxiety, our bodies respond by releasing hormones like cortisol and adrenaline, preparing us for the “fight or flight” response. While this response is crucial for survival in threatening situations, prolonged stress can wreak havoc on our physical health.
The muscles in our bodies tense up under stress, and if left unchecked, this tension can contribute to muscle imbalances and postural issues, ultimately leading to increased pressure on the sciatic nerve. Furthermore, stress and anxiety can exacerbate inflammation in the body, further aggravating sciatica symptoms.
Can Emotional Stress Cause Sciatic Pain?
While emotional stress alone may not directly cause sciatica, it can exacerbate existing symptoms. Stress triggers the release of hormones like cortisol, leading to muscle tension and inflammation, which can aggravate sciatic pain. Additionally, stress-related behaviors like poor posture or overexertion may worsen underlying conditions contributing to sciatica. Managing emotional stress through relaxation techniques and seeking support from healthcare professionals can help alleviate symptoms and improve overall well-being, complementing other treatment approaches for sciatica.
Managing Stress and Anxiety to Alleviate Sciatica
Addressing stress and anxiety is paramount for managing sciatica effectively. Incorporating stress-reduction techniques into your daily routine can significantly improve your overall well-being. Practices such as deep breathing exercises, meditation, yoga, and progressive muscle relaxation can help calm the mind and relax tense muscles, reducing pressure on the sciatic nerve.
Additionally, prioritizing self-care activities like getting adequate sleep, maintaining a healthy diet, and engaging in regular exercise can bolster your resilience to stress and promote physical and mental health. Finding activities that bring joy and relaxation, whether it’s reading a book, spending time in nature, or pursuing a hobby, can also provide much-needed relief from the pressures of daily life.
Seeking Professional Help
While self-care practices are invaluable, it’s essential to seek professional help if stress and anxiety are significantly impacting your daily life or exacerbating sciatica symptoms. Consulting with a healthcare provider can help identify underlying issues contributing to stress and anxiety and develop a tailored treatment plan.
Therapy, such as cognitive-behavioral therapy (CBT), can equip you with coping mechanisms to manage stress more effectively and change negative thought patterns that contribute to anxiety. In some cases, medication may be prescribed to alleviate symptoms and restore balance to your mental health.
Preventing Sciatica Flare-ups
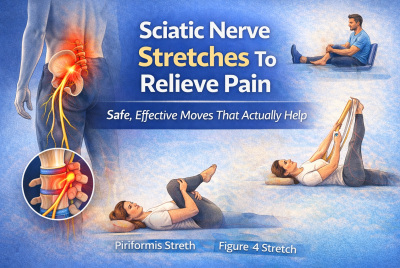
In addition to managing stress and anxiety, taking proactive steps to prevent sciatica flare-ups is crucial for long-term symptom management. Maintaining good posture, practicing proper lifting techniques, and incorporating regular stretching and strengthening exercises into your routine can help alleviate pressure on the sciatic nerve and reduce the likelihood of flare-ups.
Furthermore, being mindful of your body’s signals and avoiding activities that exacerbate symptoms can help you avoid unnecessary pain and discomfort. By prioritizing self-care and adopting healthy habits, you can empower yourself to take control of your sciatica and minimize its impact on your life.
Can Stress and Anxiety Cause Sciatica – What Lifestyle Causes Sciatica Pain?
Yes — stress and anxiety can contribute to sciatica pain, both directly and indirectly. While emotional stress doesn’t cause sciatica on its own, it can significantly worsen existing symptoms or trigger flare-ups by affecting how your body responds to pain and tension.
When you’re under stress, your body releases cortisol and adrenaline, hormones that tighten muscles and increase inflammation. Chronic tension in the lower back, hips, and glutes can compress the sciatic nerve, leading to pain, numbness, or tingling down the leg. Anxiety also alters posture — many people unconsciously clench muscles or sit rigidly for long periods, which strains the spine and aggravates nerve irritation.
Lifestyle factors that combine with stress to cause sciatica include poor posture, prolonged sitting, lack of exercise, obesity, smoking, and improper lifting habits. Together, these habits weaken the spine’s support system and increase pressure on the sciatic nerve.
In short, emotional and physical stressors often work hand in hand — managing both through exercise, stretching, relaxation techniques, and healthy routines is key to preventing or easing sciatica pain.
Frequently Asked Questions (FAQs)
Can stress alone cause sciatica?
Stress alone is unlikely to cause sciatica. While stress can exacerbate symptoms by increasing muscle tension and inflammation, sciatica typically results from physical factors like herniated discs or spinal stenosis. However, managing stress can play a crucial role in reducing the severity and frequency of sciatica flare-ups.
How can I tell if my sciatica is caused by stress or anxiety?
Differentiating between sciatica caused by physical factors and those exacerbated by stress or anxiety can be challenging. If you notice an increase in pain during times of stress or anxiety, it may indicate their contribution. Consulting with a healthcare provider can help determine the underlying causes and develop an appropriate treatment plan.
Are there specific exercises that can help alleviate sciatica-related stress and anxiety?
Yes, exercises like yoga, tai chi, and Pilates are beneficial for alleviating both sciatica-related symptoms and stress/anxiety. These activities focus on gentle stretching, strengthening, and relaxation techniques, which can help reduce muscle tension, improve flexibility, and promote a sense of calmness and well-being, ultimately aiding in the management of sciatica and associated stress.
Can medication help with both sciatica and anxiety?
Some medications, such as muscle relaxants and certain antidepressants, may be prescribed to alleviate both sciatica symptoms and anxiety. However, it’s essential to consult with a healthcare provider to determine the most appropriate treatment plan for your specific needs.
How long does it take to see improvements in sciatica symptoms with stress management techniques?
The timeline for seeing improvements in sciatica symptoms varies from person to person. Consistently practicing stress management techniques alongside other treatment methods can lead to gradual improvements over time, but it’s essential to be patient and persistent in your efforts.
Can Stress and Anxiety Cause Sciatica – Conclusion
In conclusion, while stress and anxiety may not directly cause sciatica, their impact on the body can exacerbate symptoms and make the condition more challenging to manage. By addressing stress and anxiety through various techniques and seeking professional help when needed, individuals with sciatica can significantly improve their quality of life and reduce the frequency and severity of flare-ups. It’s essential to recognize the interconnectedness of mental and physical health and prioritize self-care practices that promote relaxation and overall well-being. With dedication and persistence, managing stress and anxiety can become an integral part of effectively managing sciatica symptoms.
Disclaimer
This article is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always consult with your healthcare provider before starting a new exercise or stretching routine, especially if you have existing back or nerve conditions.
👉 Explore more: