The Hidden Link Between the Vagus Nerve and Sciatica Pain: What You Need to Know
When Sciatica Feels Deeper Than a Back Problem
If you’ve been dealing with sciatica pain — that sharp, burning, or tingling sensation that runs from your lower back down your leg — you probably assume it’s purely a spinal issue. But what if your nervous system and stress levels were also playing a role? Emerging research suggests a surprising connection between the vagus nerve and sciatica pain. This large, powerful nerve influences inflammation, digestion, stress, and even pain sensitivity. When it’s not functioning properly, it can make sciatica symptoms worse or harder to control.
Let’s explore how the vagus nerve affects sciatica and what you can do to support both for long-term relief.
What Is the Vagus Nerve?
The vagus nerve is the longest cranial nerve in the body. It runs from the brainstem through the neck and chest into the abdomen, connecting to major organs like the heart, lungs, and intestines.
Its primary role is to regulate the parasympathetic nervous system — the “rest and digest” branch responsible for calming your body after stress.
When working properly, the vagus nerve:
-
Lowers heart rate and blood pressure
-
Reduces inflammation
-
Promotes digestion
-
Balances immune function
-
Regulates mood and pain perception
But when it’s underactive or “stressed out,” your body stays in fight-or-flight mode, which can trigger chronic inflammation and worsen pain signals — including those from the sciatic nerve.
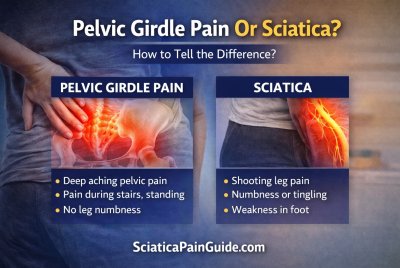
Understanding Sciatica and Nerve Inflammation
Sciatica occurs when the sciatic nerve — the longest nerve in the body — becomes compressed or irritated, often due to:
-
A herniated disc
-
Spinal stenosis (narrowing of the spinal canal)
-
Piriformis syndrome (tight hip muscle pressing on the nerve)
-
Inflammation or swelling around the lower spine
When inflammation is persistent, pain signals become amplified. That’s where the vagus nerve enters the picture — it helps regulate inflammation throughout the body, including near the spine.
The Connection Between the Vagus Nerve and Sciatica Pain
Recent studies and integrative health practitioners highlight how poor vagus nerve function can worsen sciatic pain in several ways:
1. Increased Inflammation
The vagus nerve has an anti-inflammatory pathway known as the “cholinergic anti-inflammatory reflex.” When activated, it helps suppress the production of inflammatory molecules (like cytokines) that irritate nerves.
If vagal tone is low, inflammation remains high — making sciatic pain more severe.
2. Muscle Tension and Stress Response
Chronic stress tightens muscles around the lower back and hips, increasing pressure on the sciatic nerve. An overactive stress response also elevates cortisol levels, which can inflame tissues.
A calm, active vagus nerve helps relax muscles and lower stress hormones.
3. Pain Signal Regulation
The vagus nerve communicates with the brain’s pain centers. When it’s stimulated, it can actually dampen pain signals — a process known as “descending inhibition.”
In people with poor vagal tone, pain signals can feel louder and more persistent.
4. Gut-Brain Connection
Poor digestion or gut inflammation can indirectly affect the sciatic nerve. The vagus nerve plays a major role in digestion, and when the gut is inflamed, it can raise systemic inflammation that worsens nerve pain.
Signs of a Weak or Underactive Vagus Nerve
People with poor vagal tone often experience a mix of symptoms that go beyond sciatica, including:
-
Anxiety or difficulty relaxing
-
Digestive issues (bloating, constipation)
-
Low energy and poor sleep
-
Frequent headaches or tension
-
Rapid heart rate or shallow breathing
Improving vagus nerve function can support your body’s ability to calm inflammation and manage chronic pain more effectively.
Vagus Nerve Stimulation for Sciatica Relief
Research into vagus nerve stimulation (VNS) — both medical and natural — shows promise for chronic pain conditions. Here are some safe, at-home methods to help activate the vagus nerve and possibly reduce sciatica symptoms:
1. Deep Diaphragmatic Breathing
-
Sit or lie comfortably.
-
Inhale deeply through the nose, expanding your belly for 4 seconds.
-
Hold for 2 seconds, then exhale slowly for 6 seconds.
-
Repeat for 5 minutes daily.
👉 This activates the vagus nerve and reduces muscle tension around the spine.
2. Cold Exposure (Vagus Activation Technique)
A splash of cold water on your face or neck triggers a mild shock response that stimulates the vagus nerve.
-
Try 15–30 seconds of cool water on your face each morning.
-
Or finish showers with 20 seconds of cold water.
3. Humming, Chanting, or Singing
The vagus nerve connects to the vocal cords — humming or chanting creates a gentle vibration that stimulates it.
-
Try humming for 5 minutes a few times daily.
-
Singing along to music can have the same benefit!
4. Gentle Yoga and Stretching
Certain poses calm the nervous system while easing sciatic tension:
-
Cat-Cow Stretch
-
Supine Twist
👉 Combine with slow breathing to engage the vagus nerve while relaxing lower back muscles.
5. Massage and Acupressure
Massaging areas near the neck and behind the ears can stimulate vagal pathways.
-
A professional craniosacral massage or vagus nerve-focused acupressure may enhance relaxation and nerve recovery.
6. Healthy Gut Support
A balanced gut helps reduce systemic inflammation — and because the vagus nerve controls digestion, gut health and vagal tone go hand in hand.
-
Eat fiber-rich foods, fermented foods (yogurt, kefir, sauerkraut), and omega-3s.
-
Avoid processed sugar and refined carbs that fuel inflammation.
Lifestyle Tips to Strengthen the Vagus Nerve and Reduce Sciatica Pain
Here’s how to integrate vagus support into your daily routine:
-
Practice mindfulness or meditation for 10–15 minutes per day.
-
Maintain good posture to prevent spinal compression.
-
Sleep 7–9 hours nightly to allow nerve regeneration.
-
Stay hydrated to support spinal disc health.
-
Limit alcohol, caffeine, and smoking, all of which impair vagal function.
Over time, these habits can improve your body’s ability to self-regulate inflammation and relieve pain naturally.
When to Seek Professional Help
If your sciatic pain persists beyond 4–6 weeks, or if you experience numbness, weakness, or loss of bladder/bowel control, see a healthcare professional immediately.
You may benefit from:
-
Physical therapy
-
Chiropractic adjustments
-
Anti-inflammatory medications
-
Clinical vagus nerve stimulation (used for chronic pain and epilepsy)
Real-Life Connection: Stress, Mind, and Nerve Pain
Many Americans notice that their sciatica flares up under stress. This isn’t a coincidence — stress suppresses vagus nerve function and tightens back muscles.
That’s why approaches combining physical stretches + nervous system calming (like yoga, breathwork, and mindfulness) tend to outperform physical therapy alone in long-term studies.
FAQs About the Vagus Nerve and Sciatica Pain
1. How are the vagus nerve and sciatica connected?
The vagus nerve helps control inflammation and muscle relaxation. When it’s underactive, inflammation can worsen around the sciatic nerve, increasing pain.
2. Can vagus nerve stimulation help sciatica?
Yes, some people experience relief when stimulating the vagus nerve through breathing, humming, or cold exposure, as it reduces inflammation and stress-related tension.
3. Does stress make sciatica worse?
Absolutely. Stress triggers tight muscles and inflammation that can compress the sciatic nerve. Activating the vagus nerve helps counter this response.
4. Are there supplements that support vagus nerve function?
Omega-3 fatty acids, magnesium, and probiotics may enhance vagal tone by supporting nerve and gut health.
5. How can I naturally activate my vagus nerve?
Try deep breathing, humming, cold showers, meditation, or yoga — all proven to gently stimulate the vagus nerve.
6. Can gut health affect sciatica pain?
Yes. Gut inflammation raises systemic inflammation, which can irritate nerves. Strengthening the vagus nerve improves gut function and reduces flare-ups.
7. Should I see a doctor for vagus nerve-related sciatica?
If your symptoms are severe or persistent, consult your doctor or physical therapist. They can identify whether nerve compression, inflammation, or stress is the root cause.
Conclusion: Healing Sciatica from the Inside Out
Your vagus nerve and sciatic nerve might seem unrelated, but they share one thing in common — both are deeply affected by inflammation and stress.
By supporting your vagus nerve through breathing, relaxation, and mindful living, you can help calm your entire nervous system and naturally reduce sciatic pain. Combine these habits with stretching, posture care, and medical guidance, and you’ll be taking a whole-body approach to recovery — not just masking pain.
Disclaimer
This article is for educational purposes only and is not a substitute for medical advice, diagnosis, or treatment. Always consult your healthcare provider before starting any new therapy or exercise related to sciatica or nerve health.

- Yoga Poses to Avoid with Sciatica
- Top 10 Foods to Eat If You Have Sciatica
- Sciatica Relief Stretches for Beginners